International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Mini Review - (2024)Volume 12, Issue 6
Vestibular disorders induce ocular motor, posturo-locomotor, perceptive, and cognitive disorders that are severe handicaps for patients in their everyday life, and they significantly reduce their quality of life. Animal models of unilateral vestibular loss showed that the vestibular syndrome was composed of both static and dynamics deficits which compensation was achieved by different recovery mechanisms. While the static deficits oberved in stationary animals resulted from the imbalance between the Vestibular Nuclei (VN) on both sides, and their compensation by the restoration of the electrophysiological homeostasis in these nuclei over time, the dynamic deficits found in active animals moving head and body in space were poorly recovered and required the whole brain to elaborate new strategies, new learned behaviors. How does Vestibular Rehabilitation therapy (VR) influence and affect the recovery of the vestibular functions remains however poorly documented in the literature in both animal models and patients with acute vestibular loss.
Vestibular disorders; Vestibular Rehabilitation Therapy (VRT); Spontaneous Neural Activity (SNA); Subjective Visual Vertical Test (SVVT); Acute Unilateral Peripheral Vestibular Pathology (AUVP)
Patients with Acute Unilateral Peripheral Vestibular Pathology (AUVP) exhibit the same deficits as those reported in animal models [1]. The static deficits are defined as the ocular tilt reaction, an eye-head synkinesis in the roll plane that include conjugate ocular torsion, skew deviation, head and body tilt, and Subjective Visual Vertical (SVV) offset to the hypofunction side [2,3]. There is a slow spontaneous compensation that takes 6 months to 1 year, depending on the patients and on the nature of the static deficits [4]. The main compensation process for the static deficits is based on the re-expression of developmental plasticity mechanisms in the deafferented VN, rebalancing the spontaneous neural activity on both sides, and inducing neural protection and structural reorganization [1,5]. On the other hand, impairment of gaze stability and dynamic balance control, the dynamic counterpart of the vestibular syndrome, are compensated for by newly elaborated sensory and behavioral strategies implicating a large neuronal network (thalamus, tempoparietal cortex, cerebellum) [1,5].
Vestibular Rehabilitation therapy (VR) is commonly used by specialized physiotherapists to improve the patient’s quality of life, and to speed up the compensation process. The Cochran database of systematic reviews indicate that there is moderate to strong evidence that VR is a safe, effective management for unilateral peripheral vestibular dysfunction, based on a number of high quality randomized controlled trials [6,7]. A review paper we recently published pointed to the strong interaction between Vestibular Compensation and VR [8]. Our recent clinical investigations have questioned the impact of VR on the compensation process, and we tried to know why, how and when VR must be done. They were also aimed at testing and validating different VR protocols used by physiotherapists in their routine practice.
Effectiveness of VR was assessed by comparing AUVP patients with and without VR examined at the same time period after symptoms onset. The clinical investigations reported in the present mini review included rehabilitated patients who received early VR (first two weeks after onset) and two VR sessions per week, till complete compensation (one month on average), and non-rehabilitated patients in whom the spontaneous compensation was also tested one month after symptoms onset. Recovery of the static and dynamic vestibular functions was assessed with different VR protocols and outcomes.
The balance deficits were analyzed with static (Stable support: Easy condition) and dynamic (Unstable support: Challenging condition) posturography in different visual conditions (eyes open, eyes closed, with optokinetic stimulation) and non-linear analysis of the stabilogram (wavelet analysis). The ocular motor deficits were assessed by the spontaneous nystagmus recorded in darkness and the asymmetry and directional preponderance of the angular vestibulo-ocular reflex. The perceptive deficits were investigated using the Subjective Visual Vertical (SVV) test that evaluates the bias in the perception of verticality.
Different VR protocols were tested. The rotatory chair paradigm consisted in repeated whole body rotations towards the disease side. It was used to symmetrize the vestibular responses from the healthy and weaker sides. Gaze stability exercises included fast motion of the head in the planes of the three semicircular canals in order to recover the dynamics of the canal function and/or to favor compensatory saccades. Finally, the tilted support protocol was used to normalize the SVV. This new rehabilitation tool consisted in training patients to stand quietly with eyes open and eyes closed on an inclined support towards the side of the SVV bias and with the same amplitude than the SVV bias, in order to induce postural corrections away from the SVV bias (see for details the original papers).
Figure 1 illustrates the mean values of the static vestibular deficits recorded in the AUVP patients before (open histograms) and after (black histograms) VR, at the end of the rehabilitation sessions, together with the data collected at the same time period after symptoms onset in AUVP patients without VR (grey histograms).
Posturography recordings of posture performance in easy conditions (eyes open and stable support) and data processing with non-linear analyses of the stabilogram, showed significant reduction of the postural instability index (Figure 1A) and of the energy cost to maintain balance (Figure 1B). A faster normalization of both postural parameters was found in the patients rehabilitated with the rotatory chair protocol compared to the spontaneous compensation observed in the patients without VR [9]. SN normalization took 90 days on average without VR, and 14 days with the rotatory chair rehabilitation, that is, a hazard ratio of around 15 times the rate of SN normalization in patients with spontaneous SN compensation. Non-pathological SN values (<2°/s) were found at the end of the VR sessions (around one month) in the rehabilitated patients while the patients without VR still exhibited pathological values above 2°/s at the same time period [10]. Normalization of the Subjective Visual Vertical (SVV) was investigated in another set of experiments using the tilted support protocol [11]. Results at this perceptive level again showed a faster SVV normalization in the rehabilitated patients (3-4 weeks) compared to the spontaneous normalization in the patients without VR (Figure 1C), for whom SVV normalization required much more time (3-6 months). Moreover, a close temporal correlation was observed between SVV normalization and posture normalization, suggesting a close link between the perception of body orientation in space and the control of body position in space. Recordings of the Spontaneous Nystagmus (SN) in darkness showed similar findings (Figure 1D).
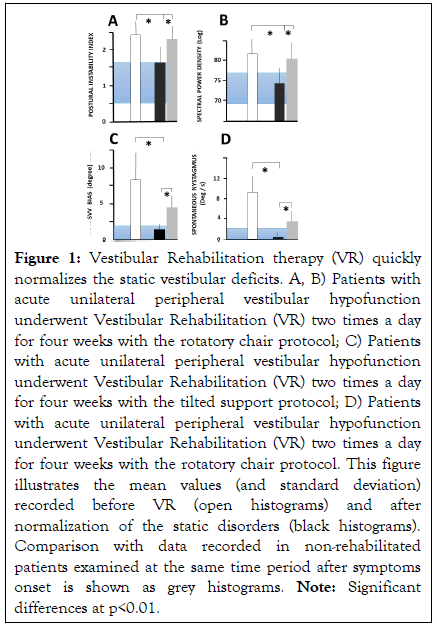
Figure 1: Fourty-nine c with ATTR-CM were compared with matched control with atrial fibrillation, showing that ATTR-CM is characterized by increased inflammation and an unbalance in ECM homeostasis, with degradation prevailing over synthesis of ECM.
A): Normalization of the postural instability index provided by the wavelet analysis of the stabilogram. This postural parameter recorded in eyes open condition on a stable support was significantly increased in the patients tested before VR compared to healthy participants in the same class of age (blue area indicating the range of the control values). At the end of VR (around one month after symptoms onset), body stabilization regained control values whereas the spontaneous compensation observed at the same time period in the non-rehabilitated patients remained in the pathological range, B): Same presentation with the spectral power density also derived from the wavelet analysis, indicating that rehabilitated patients spent less energy to control their posture compared to non-rehabilitated patients, C): Normalization of the Subjective Visual Vertical, the perception of verticality performed with the adjustment test to the true gravitational vertical in patients without orienting visual cues. The normal range is plotted as the blue areas (<2 degrees), (D): Normalization of the spontaneous nystagmus recorded in darkness. Non-pathological values (<2 degrees/s) are plotted as the blue areas.
The comparison of early (first two weeks) versus delayed (thirdfourth week) or late (three months) VR with the different protocols always led to normalization of all the static postural, ocular motor and perceptive deficits. There is no true critical period to compensate the static deficits, but earlier is better to quickly normalize the static deficits.
By contrast, the compensation of the dynamic vestibular deficits is highly dependent on the time passed between symptoms onset and the start of rehabilitation. Posturography recordings in more challenging conditions (eyes closed, unstable support) clearly showed that VR with the rotatory chair protocol or gaze stabilization exercises led to optimal compensation when performed early after symptoms onset [12]. Similar findings were found for the recovery of dynamic visual acuity [13]. This earlier is better concept corroborates the critical period we highlighted in animal models of unilateral vestibular loss. Early rehabilitation is a necessary but not sufficient condition, however, to recover the dynamic vestibular functions: the degree of vestibular loss matters [14-17].
The positive outcomes of VR with the rotatory chair protocol, that is, repeated whole body rotations to the hypofunction side, are very likely based on the rebalance of neuronal activity in the vestibular nuclei and the regain of symmetrical spontaneous resting discharges on both sides. This recovery mechanism is commonly reported in the literature to explain the compensation of the static vestibular deficits. Such symmetrization could result from the habituation of the contralateral healthy side response, inhibited by the repetition of the stimulations, and from the stimulation of remaining intact vestibular afferents on the weaker side. The tilted support protocol likely reweights the visual and somatosensory cues involved in the perception of verticality. A shift to a reference frame based on body in space orientation seems to be used to recalibrate the perception of verticality and to restore the orientation constancy. The gaze stabilization exercises are active head movements favoring the adaptation processes and the elaboration by the whole brain of new strategies substituting to the defective vestibular functions.
Different VR protocols interfere with the plasticity mechanisms participating in the recovery of the static and dynamic deficits, and brain plasticity-based therapeutics are the way to normalize the defective vestibular functions. The crucial messages for optimal vestibular function recovery are: 1) VR should not be stereotyped and based on a single rehabilitation protocol, 2) static deficits in humans are compensated within a much longer time period compared to animal models. VR is therefore a good opportunity to significantly shorten the recovery time course and regain quickly a good quality of life, 3) The recovery of the dynamic vestibular functions such as gaze stabilization and balance requires to perform VR during the early critical time window of high neuronal plasticity. This early period constitutes an opportunity window for physiotherapists, 4) VR protocols based on active retraining, adaptation and substitution processes, customized for each patient, favoring ecologic contexts, reducing anxiety and increasing motivation should be the common sense principles to regain the best quality of life.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Lacour M, Haijoub S (2024) Vestibular Rehabilitation Normalizes the Impaired Vestibular Functions. Int J Phys Med Rehabil. 12:738.
Received: 01-Jul-2024, Manuscript No. JPMR-24-32543; Editor assigned: 04-Jul-2024, Pre QC No. JPMR-24-32543; Reviewed: 18-Jul-2024, QC No. JPMR-24-32543; Revised: 25-Jul-2024, Manuscript No. JPMR-24-32543; Published: 31-Jul-2024 , DOI: 10.35248/2329-9096.24.12.738
Copyright: © 2024 Lacour M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.