
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2022)Volume 12, Issue 4
A 33-year-old woman was admitted to the hospital due to a sudden cardiac arrest. After admission, she presented with polymorphic ventricular arrhythmia, broad QRS complexes, and severely impaired left-ventricular function. A glass container with conifer needles was found in the personal patients’ belongings; the therapy was adapted to possible oral intoxication. Fortunately, hemodynamics stabilized. After extubation, the patient confirmed oral intake of yew needles to experience narcotic effects. Yew (Taxus baccata) intoxication is rare and mostly associated with suicidal attempts. The presented case describes the first-time oral yew intake as a narcotic drug and may help physicians to detect potential abuse.
Yew; Intoxication; Extracorporeal Membrane Oxygenation (ECMO); Extracorporeal Life Support (ECLS); Cardiogenic shock
Yew (Taxus baccata) is widely spread as an ornamental plant and is associated with cases of intoxication and suicidal attempts (Figure 1) [1,2]. Yew contains taxin B, affecting the atrioventricular conduction system. The cardiotoxic effect is triggered by calcium channel (ICa) and a fast cardiac sodium channel (INa) blockade. Yew intoxication causes nausea, vomiting, and abdominal pain associated with cardiac arrhythmias, unconsciousness, and respiratory insufficiency. Yew consumption aiming for narcotic effects is rare and difficult to detect.
Figure 1: Yew needles of Tacus baccata.
A specific antidote is not available and therapeutic concepts are limited. Therefore, we present our interdisciplinary experience with a 33-year-old woman who survived yew intoxication. Additionally, we report on the potential novel usage of yew as a narcotic drug and discuss all relevant aspects of intoxication with Taxus baccata.
A 33-year-old woman self-contacted the local Emergency Medical Services (EMS) due to general discomfort. Upon the arrival of the EMS the patient complained about dizziness and nausea; the patient denied having any previous diseases, pregnancy, and any medication or substance abuse. Due to sudden loss of consciousness, orotracheal intubation was performed. Electrocardiogram (ECG) showed a broad complex tachycardia (Figure 2) and blood pressure was 60/30 mmHg with a need for inotropic support; however, the patient showed further hemodynamic instability, and Cardiopulmonary Resuscitation (CPR) was started. Pharmacological therapy with amiodarone was initiated and multiple attempts of electrical cardioversion were inefficient to terminate the tachycardia. In regard to standardized protocol, 250 mg acetylsalicylic acid and 5000 IU heparin were administered preclinically.
After initial hospitalization, coronary angiography did not show any coronary vascular disease. However, laevocardiography revealed a severely impaired left ventricular ejection fraction, additionally confirmed by Transthoracic Echocardiography (TTE), with signs of an asynchronous contraction pattern and hypermobility of the septum. Hemodynamic instability persisted with the need for CPR and intermittent Return Of Spontaneous Circulation (ROSC). ECG constantly revealed various abnormalities, including asystole, total AV-block, and polymorphic ventricular tachycardia. An external temporary VVIpacemaker was placed transvenously into the right ventricle ( Figure2).
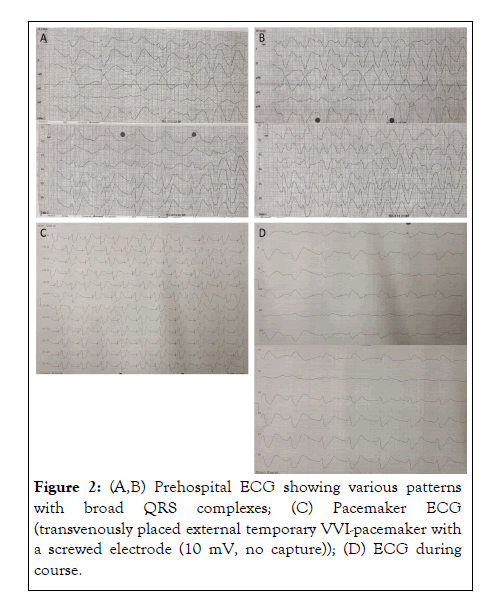
Figure 2: (A,B) Prehospital ECG showing various patterns with broad QRS complexes; (C) Pacemaker ECG (transvenously placed external temporary VVI-pacemaker with a screwed electrode (10 mV, no capture)); (D) ECG during course.
The ECMO center was contacted for potential Extracorporeal Life Support (ECLS) and retrieval to the hospital. In the meantime, the hemodynamic situation stabilized. A head, thorax, and abdomen CT scan showed no abnormalities. The patient was finally transported to the ECMO center with ECMO stand-by for further diagnostics. Hemodynamics was maintained by amiodarone, and high dose of inotropic and vasoactive support. However, continuous stimulation by the external pacemaker was necessary. Blood samples were analyzed showing low potassium levels (3.1 mmol/L), and elevated liver enzymes (GOT 161 U/L, GPT 152 U/L). The LDH accounted for 382 U/L, and the neutrophilic count was 7820 per μL (79%). Lactate peaked at 2.8 mmol/L. Importantly, the patient ´s personal belongings included a preserving jar with partly chopped conifer needles (Figure 3).
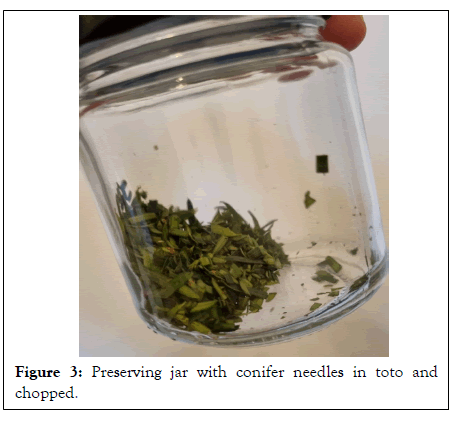
Figure 3: Preserving jar with conifer needles in toto and chopped.
In cooperation with the responsible poison center, the needles were identified as yew (Taxus baccata), and underlying symptoms were discussed due to a potential intoxication. Due to the potential oral intake, gastric draining was performed, and charcoal medication with laxatives was administered. However, the presence of yew needles in the aspired gastral secret could not be verified, so the diagnosis could not be confirmed by the presence of yew needles in the patient’s stomach. Thereafter the patient continuously stabilized under ongoing reduction of vasoconstrictor and without ECMO therapy support. Twentyfour hours after initial hospital admission, the ECG normalized showing a norm frequent sinus rhythm. The Patient was extubated thirty-six hours after the initial admission, showing a total recovery of left ventricular ejection fraction. The patient confirmed the oral intake of yew leaves, still negating a suicidal attempt. Her supposed intention of oral intake was based on a crime novel and the demand for self-experience of the low-dose narcotic effect. Except for recurrent vertigo, no specific symptoms in the first hours after intake of the yew leaves were evident for the patient.
Following psychiatric diagnostics revealed no acute risk of suicide or potential psychiatric disorders. After three days, the patient was discharged in a stable hemodynamic condition. Blood and urine samples were collected about 8 hours after initial hospitalization. Analyses were performed at the Institute of Legal Medicine in Dresden (Germany) as described elsewhere [3]. In brief, 0.5 mL of blood and urine were extracted by liquid/ liquid extraction and separated by High-Performance Liquid Chromatography (HPLC) using a Luna Pentafluorophenyl (2) 100 Å (150 mm × 2 mm, 5 μm) column from Phenomenex (Aschaffenburg, Germany). Using a 3200 QTrap® from AB Sciex (Darmstadt, Germany), generally following analytes could be identified within this method (Limits Of Detection (LOD) are given in brackets): 3, 5 Dimethoxyphenol (LOD 5 ng/mL), 10- Deacetylbaccatin III (LOD 5 ng/mL), Baccatin III (LOD 5 ng/ mL), Cephalomannin (LOD 0.5 ng/mL), Taxinin M (LOD 0.5 ng/mL), Taxol A (LOD 0.5 ng/mL).
In blood as well as in urine samples, only taxinin M could be identified and quantified. The concentrations were 3.8 ng/mL and 2.0 ng/mL, respectively.
Taxus baccata-geobotany, phytomorphology and toxicity
The toxicity of yew plants is related to taxines, which can be found in all parts of the plant except the scarlet aril [4]. Consumption of the red and fleshy seed coat causes mild symptoms such as nausea, vomiting, or skin reactions, whereas intake of yew needles is far more dangerous [5]. Yew has its highest poison content in winter [6]. The lethal dose for an adult corresponds to 50 g of yew needles, accounting for 250 mg taxus alkaloid or approx. 3 mg taxine per kilogram body weight [6,7]. Consumption of crushed or chopped yew needles, as described in our case, results in five times higher concentration of taxine degradation products in the blood than consumption of intact needles [8].
Background of yew poisoning
Yew intoxication is a common method of suicide [9]. Besides the well-known use for the suicidal purpose, some reports indicate relatively frequent incidental intake by children, mainly due to the temptation to taste the red arils. In regard to provided data by the Toxicological Information Service in the Czech Republic, approximately 60% of consulted patients (study period from 2005 to 2014) were children younger than 3 years [10]. In the early 2000s in Dresden, Germany, a case series of five young adults with fatal taxus poisoning was described. Due to the lethal outcome, possible drug abuse couldn’t be confirmed, and a suicidal intake was presumed [9]. So far, reports about yew intake as a party drug or for narcotic purposes are lacking in current literature. As described in our case, the patient’s purpose was to experience a low-dose narcotic effect triggered by crime novel description. In online user blogs, the use of yew as a ‘psychonautic’ agent is described [11]. The application as an ingredient of incense is recommended there, whereas a warning is given of oral intake and smoking due to the high content of alkaloids.
Pharmacokinetic and specific symptoms of oral yew intake
The two taxines, taxine A (C35H47NO10), and taxine B (C33H45NO8) of Taxus baccata, are toxic alkaloids [6]. The cardiotoxic effect is triggered by taxine B, inhibiting heart muscle cells by a calcium channel (ICa) and a fast cardiac sodium channel (INa) blockade [5,6,8]. Blocking the sodium channels leads to a widening of the QRS complex and ventricular arrhythmias (ventricular tachycardia or ventricular fibrillation). Blocking of calcium channels results in bradycardia and atrioventricular block, reduced myocardial contractility, and arterial hypotension.
Initially, this causes light symptoms such as nausea, vomiting, and abdominal pain. Shortly after, it leads to severe cardiac arrhythmias, unconsciousness, respiratory insufficiency, and in the worst death case. Retrospectively, described symptoms were evident in our patient. In in-vivo animal experiments, a high concentration of taxine B (5 μM) increased atrioventricular conduction and widened QRS intervals. A lower concentration (1 μM) results in a significantly reduced heart rate [12]. Intake of taxine B leads to atrioventricular conduction blocks and complete diastolic cardiac arrest. Also, the effect of taxine B resembles the action of class I antiarrhythmic drugs (e.g., flecainide, verapamil, quinine) [13]. Taxine A induced only mild reductions in heart rate [12].
Diagnostics of yew poisoning
Acute yew intoxication is hard to diagnose. After exclusion of more common cardiac causes, the cardiac dysrhythmias with the appropriate wide complex QRS complexes, varying between bradycardia and tachycardia, as well as a prolonged QT interval or a broad and peaked T wave combined with respiratory insufficiency or failure are pathognomonic signs. Intoxication with other antiarrhythmic or antidepressant drugs leading to QRS widening should also be considered [14-16]. The additional presence of yew needles in gastric secret should make physicians aware of potential oral yew intake.
Since taxine B, the most toxic component in yew, is unstable and thus difficult to detect in post-mortem blood [5], several yew components are used to prove an intoxication with yew, e.g., baccatin III, 10-Deacetylbaccatin III, Taxine B, Isotaxine B, (Taxol A), Cephalomannine (Taxol B) and 3, 5 Dimethoxyphenol (3, 5- DMP) [8]. The detection of 3, 5- DMP is quite common to indicate a yew intoxication, even though it is not specific to yew [17]. However, post-mortem 3, 5-DMP concentrations in body fluids and organs were reported in the literature to confirm the preliminary diagnosis of taxus intoxication. Especially the concentrations in cardiac blood samples showed a wide range between 31 ng/mL and 110 ng/ mL, which most probably is due to the form of ingestion. An outstanding concentration of 528 ng/mL in cardiac blood and 118 μg/g in stomach content underline the possible distinct effect of Postmortem Redistribution (PMR) [9].
There are very few reports of suicide attempts by yew intoxication, since the poisoning is usually fatal without immediate medical intervention. Kobusiak-Prokopowicz M, et al. [18], reported a case of a patient found unconscious, who admitted consuming yew leaves after recovery. In the patient’s blood serum, 3, 5-DMP and Taxine B/Isotaxine B could be identified [18].
Neither in the blood, nor the urine sample of the presented patient 3, 5-DMP could be detected. Only the taxus component taxinin M was identified. This most probably is based on the comparably low dose of yew leaves ingested and the period between ingestion and the collection of the samples.
Therapy
There is no specific treatment for intoxication with yew needles. Emergency medical care following Intensive Care Unit (ICU) admission mainly aims to avoid or treat related symptoms or complications. In case of suspected yew poisoning, a gastroscopy and charcoal should be administered immediately [19]. Since needles are passing the gastrointestinal tract slowly, gastric drainage is recommended even several hours after ingestion [1]. In addition to gastroscopy and the administration of medical charcoal, fat emulsions may be administered off-label due to recent literature [20].
In some cases of yew intoxication, increased digoxin levels have already been demonstrated [5,21]. This is most likely due to a cross-reaction of digitalis and yew alkaloids [5]. This finding might suggest the potential benefit of anti-digoxin antibody administration [19].
In case of long-lasting polymorphic arrhythmias, treatment with antiarrhythmic drugs such as amiodarone or defibrillation are recommended. For bradyarrhythmia, external or internal pacing of the heart should be performed. Taxine B cannot be removed by hemodialysis due to its high molecular weight and low solubility. However, in cases of severe metabolic disorders, hemodialysis should be implemented additionally [22].
ECMO therapy in patients with severe cardiac failure due to yew poisoning
In the initial phase of yew intoxication, when diagnostics are not completed, several reports are presented and emphasize the implementation of ECMO support due to severe cardiac failure [23]. Hermes-Laufer J, et al. [23], and colleagues recently summarized their experience with two yew poisoned ECMO patients and conducted a literature review of additional 9 patients. They reported on promising hypoxic-brain-damage-free survival of 72% (8 of 11). In general, ECMO therapy in poisoned patients is rarely performed. However, Wang GS, et al. [24], and his colleagues corroborate the findings by Hermes- Laufer with their review of the Toxicology Investigators Consortium that ECMO support can be a bridge to recovery in poisoned patients [24].
As presented in our case, recurrent cardiac arrest and severely impaired ventricular function necessitated potential Extracorporeal Life Support (ECLS), and following therapy in a center with Extracorporeal Membrane Oxygenation (ECMO) standby support. The presented case describes the first-time oral yew intake as a narcotic drug and may help physicians to classify underlying specific symptoms and to detect potential abuse of this plant. The presentation in mass-media of such suicide methods and the widespread of yew trees in our geographic area, together with the quick lethal effects through the cardiac arrhythmias, make the Taxus baccata poisoning extremely accessible.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Suhr L, Djordjevic I, Juebner M, Pietsch J, Eghbalzadeh K, Gaisendrees C, et al. (2022) Yew (Taxus baccata) Intoxication due to Narcotic Self-Experience Purpose: Case Report and Literature Review. J Clin Toxicol. 12:521.
Received: 20-Sep-2022, Manuscript No. JCT-22-19291; Editor assigned: 22-Sep-2022, Pre QC No. JCT-22-19291 (PQ); Reviewed: 06-Oct-2022, QC No. JCT-22-19291; Revised: 13-Oct-2022, Manuscript No. JCT-22-19291 (R); Published: 20-Oct-2022 , DOI: 10.35248/2161-0495.22.12.521
Copyright: © 2022 Suhr L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.